AMA President Dr Omar Khorshid press conference - Tasmania Hospital Report Card and Stop the Logjam campaign
Transcript: AMA President Dr Omar Khorshid press conference launching the AMA’s Tasmanian Public Hospital Report Card. Outside Launceston Hospital, 17th March, 2022.
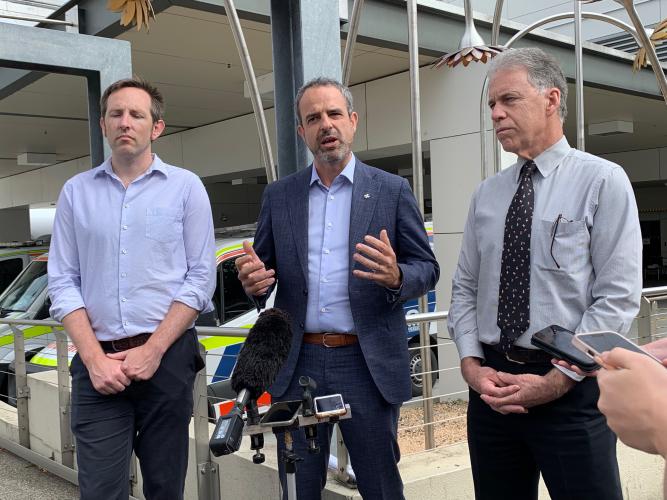
OMAR KHORSHID: Thank you everybody for coming today. My name's Omar Khorshid, President of the Australian Medical Association, and I'm joined today by Dr Glenn Richardson, who's the chair of the AMA Tasmania Council, and Dr Jerome Muir Wilson, who's a GP here in Launceston.
Tasmania continues to languish at the bottom of the performance of our states and territories when it comes to public hospital performance, particularly in the area of elective surgery where only just over a third of patients who need their surgery within 90 days are actually getting it within that recommended timeframe. So the majority are waiting too long, and longer than has been suggested by their doctors.
OMAR KHORSHID: We've also seen terrible figures when it comes to access to emergency care, with Tasmanians waiting too long when they attend an emergency department. And only around 50 per cent of patients are receiving care within half an hour, for urgent category three patients attending the emergency department. And those are people with severely painful conditions, major broken bones, things that really need to be dealt with rapidly.
Even worse, at the Royal Hobart Hospital, if you go there with an emergency condition that should be dealt with within 10 minutes, under 50 per cent of patients are actually dealt with within that timeframe. And of course time is critical when it comes to those urgent conditions, and a delay can mean a far worse outcome for that patient.
So we're here today also to talk about solutions. The AMA unfortunately is tracking the worst public hospital performance right across the country, and we think therefore that this is a national problem, and we need a national solution. We have a federal election coming up, and we are calling on government - whoever forms government - to commit to spending more money on public hospitals and evenly sharing that funding with our state governments. At the moment, the Federal Government pays for 45 per cent of public hospital funding; we think it should be 50 per cent, and that extra money should be reinvested by our state governments into public hospitals.
We're also asking state governments to commit that extra 5 per cent, and if it does come from the Federal Government that it will stay in health and it will not be taken out to other parts of government expenditure. That is absolutely critical, and I've written to all the health ministers seeking that assurance. Yesterday, I got that assurance from the health minister of South Australia and also from the Opposition leader, coming up to their election on Saturday, and I'm seeking the same from the Tasmanian government.
The AMA is running a Clear the Hospital Logjam campaign, and the idea behind that is to demonstrate to the public, as we come up to the election, that hospitals are in crisis and they are jammed up. The reason there are so many ambulances, as you see behind me, that can't offload their patients into the emergency department, is that the emergency department’s full. The reason the emergency department is full is because they can't get their patients off into the ward. The ward is full because there are too many patients on the ward, there's not enough beds, and also because the back door is jammed up as well, with the hospitals unable to get their patients who've recovered enough to leave hospital back out into aged care or into disability care. So the whole thing's jammed up, and we need a national solution. And in our mind, the national solution will be found with greater funding of public hospitals and a greater Commonwealth commitment, along with a commitment from the states to reinvest in health care.
Now of course, here in northern Tasmania we have a couple of key marginal seats that are of critical importance as we go to an election. And while I'm here in Launceston, I'll be meeting with three of the four candidates for election, including Bridget Archer, the sitting member in Bass, and the two Labor candidates for Bass and Braddon. And I'll be asking them to make a commitment. What do they feel about 50-50 funding? Will they be pushing their parties to come to the rescue for hospitals, like Launceston General behind me, which are just too small to deal with the demand that they're being asked to do? So I'm really hoping to get some firm commitments from them so that people, the voters in those key marginal seats, know where their candidates stand when it comes to supporting public hospitals and health care generally here in Tasmania.
I'd like to hand over now to Dr Richardson to talk about some specifics around hospital performance here in Tasmania.
GLENN RICHARDSON: If you look behind us, you can see we've got an ED- sorry, an ED that's in crisis. Every day, 140, 150 more people end up in our emergency department. A good 30 are admitted and they have nowhere to go. We have nurses who are spending all day looking after admitted patients and not seeing the next emergency patient. This is a great little hospital. It's typical of our regional and metropolitan hospitals - It's just two thirds the size it needs to be. And we've got a tsunami of ageing patients, we've got a tsunami of diseases that go with them, and we need to somehow fix this.
If I could make a plea, when you're voting on voting day, please make health one of your big issues. Because every three years it gets talked about, and yet somehow it disappears in the campaign in the last week or two as an issue. It's got to be one of the number one things, I'm afraid.
QUESTION: What are key areas that you think Tasmanian hospitals are underperforming in?
GLENN RICHARDSON: First of all, what you see behind us is the access to our emergency department. It's choked up. We have ambulances backed up; they can't get their patients out. Doctors are left trying to see people in closets, in corridors, on seats. That's very hard to examine a patient there. Secondly, our elective surgical staff - we've got wonderful staff, but they're being asked to do more and more in less and less time, and you just cannot get through it. So our elective surgical lists in this state go up by 6000 a year. The number of people waiting to get into our specialist clinics goes up by 4000 to 6000 a year. We just can't keep up with the pace unless we increase the size of the health that we're giving to the patients.
QUESTION: Humans are definitely at the centre of this. And I noted in the report - it said, some of the people have life-threatening illnesses or injuries and are not being seen within a recommended time. Can you sort of talk me through what that means in terms of that person?
GLENN RICHARDSON: I would say that in this hospital and certainly all the hospitals in this state, if you've got such a life-threatening emergency you might die, you will be seen and you will be looked after. We do that very well. It's the next level down. They're pushed to the side because we're so busy dealing with the really difficult stuff. So some people sit outside with bleeding issues or fractures or an abdominal pain and they're waiting and they're waiting, and they're waiting longer than they should be. And that's just a capacity issue. As Omar said, if we can get another 5 per cent and undo that cap on funding, we can increase the capacity of the system and people can be seen on time and fixed up and get the appropriate treatment.
QUESTION: There would be a level of discomfort, I'm sure, with having a fracture or some sort of bleeding and being left to sit there and wait.
GLENN RICHARDSON: Yes.
QUESTION: What sort of- you know, what are nurses and doctors telling you? Are they getting, you know, people that are quite anxious, verbally abusing them?
GLENN RICHARDSON: Yep. So, first of all, with the staff, they're under enormous pressure. They are really wilting at times under this huge load. And for the poor patients they're trying to serve, they're doing their absolute best, working flat out, sometimes missing out on their own breaks or meals just to service what's going on. The patients, for the most, understand, but there are some people who get very frightened or anxious or confused and sometimes there is some degree of anger and abuse about it and that is something we just can't have. But one could argue if you've got the funding to look after people on time that would not be happening.
QUESTION: If staff members are being overworked, are they staying in the job?
GLENN RICHARDSON: Some are moving on. Yeah. We are having people who can't just keep up the pace, who are in tears at the end of a double shift because they had to stay back. That is something that's happening, yes.
QUESTION: Jeremy Radcliff has said the surgery waiting list is improving and will improve. Is that something that you are seeing? It sounds like you're seeing the opposite.
GLENN RICHARDSON: No, we're not seeing that yet. I hope he's right. But what we're seeing at the moment is more people going on the list than coming off. We're aware that COVID set us back a little bit, but we're really looking to ramp up and that's the problem. We've got that funding crisis. Surgical beds are scavenged to look after medically admitted patients. So surgeons have lists trimmed or cut because we're too busy looking after the tsunami we've got of aged, unwell patients.
QUESTION: So the 10-year plan for the LGH master plan, that's in the process now. Is it going to be- going to get worse before it gets better? And when that plan is completed, is it going to make the hospital what it needs to be?
GLENN RICHARDSON: Yeah. So first of all, I'd like to say 10 years is just too long. And I understand the State Government's got financial constraints, but our problem is we need that now in the next few years. I've seen the plan released today. It isn't just building a building, it's staffing the wards as well, so that we've got the doctors and the nurses and the physios to look after the patients. So we need additional funding, and we need it now, and the only place that can come from is a greater federal commitment to health in Australia.
QUESTION: To remove that bed block that you're talking about, do we need more services on top of the facilities they're building? They said they're going to create 12,000 square metres of additional space, but they haven't outlined all the services that they're going to provide. And Tasmanians need things like hospice care, palliative care, chronic pain services, and more maternity services. Is that something that you would expect the Government to answer?
GLENN RICHARDSON: I didn't see it in the press release, which was only made available today, I think. So I can't answer that. But we would hope, yeah, that that would be part of it. There is the efficiency question of being able to get patients out of the hospital who don't need to be there anymore, but they're waiting for placement in nursing homes, or they need rehabilitation or some other service. How do we get them out? And what you see behind you into the hospital becomes a real problem.
QUESTION: We've been hearing from Tasmanians who can't get into their GP clinic for weeks, so have to resort to going to their nearest hospital for minor treatment or medication. Is the GP shortage putting more demand on the hospital system?
GLENN RICHARDSON: Yes, it is, yeah. We have a real shortage of GPs in Australia. People would argue in places they're maldistributed, but in general, we've got a real shortage. Patients are waiting in some places up to four weeks for routine appointments. Not quite as bad in the centre here of Launceston, but people do wait. GPs can provide a lot of services to keep people out of hospitals, but they're not funded to do it.
QUESTION: Launceston General Hospital has just been the subject of another adverse finding by the Tasmanian Coroner. I think that's about the third in recent months. How can patients of this hospital have confidence that they're going to be looked after in an appropriate way?
GLENN RICHARDSON: Yeah, I haven't seen that report, so I don't know the details. But this hospital functions in extremely high level. People can definitely have confidence in the staff at this hospital. Our ED's staff are magnificent in this place.
QUESTION: One woman was advised to take her husband to the ED at the Royal Hobart Hospital to get antibiotics because he couldn't get into a GP. Are hospitals seeing more of these types of cases?
GLENN RICHARDSON: That's an unusual thing, I would have thought. I don't know the details of that case, why the person needed antibiotics. It may have been a serious condition that needed hospital, or it could have been a simple urine infection perhaps. So the lack of GP services there is the worry. Yeah.
QUESTION: With the question of funding, do you think a new million-dollar stadium for the state is an appropriate use of funds when we have a hospital system that is really crying out for help?
GLENN RICHARDSON: From a pure health point of view, no. Look, we wouldn't be pushing for a new stadium as much as we'd like to see AFL played in Tasmania and have our own team. We've got a crisis in health at the moment. This has been brewing for a long time. It's been going back 20 years. We knew this was going to happen with the demographics of the population, and we just have always been three or four steps behind and the crisis is really hitting now. We need more money, more hospital beds, more facilities for our ageing, chronic, multi-diseased population. It was always going to happen.
OMAR KHORSHID: All good? Everyone happy? Excellent.



