The burden of chronic wounds in Australia

It is widely acknowledged that chronic wounds represent a significant health and economic burden in Australia.
It is estimated that approximately 450,000 Australians currently live with a chronic wound, costing the health system around $3 billion a year.
While this burden should place wound management at the forefront of health policy decisions in Australia, chronic wounds remain an underfunded, poorly understood, and under-recognised public health issue in Australia. This is in part due to the lack of national data on the incidence and prevalence of chronic wounds in Australia and the impact on the healthcare system and the economy more broadly.
The absence of reliable and comparable data on chronic wounds has resulted in a lack of awareness about the significance of the chronic wound problem in Australia amongst policy makers, healthcare providers, and the public.
Most chronic wounds are managed in the community as opposed to hospital settings, with general practices playing a key role in the prevention, monitoring, and management of chronic wounds. Poor management of chronic wounds results in prolonged healing times, infections, long-term complications, amputations, and hospitalisations, which creates a significant physical and financial burden on patients and places pressure on an already struggling healthcare system.
The AMA estimates that the cost of hospital admissions due to chronic wounds in 2019-20 alone was $352 million, with procedures performed on chronic wounds costing $115.7 million.

The cost of hospital admissions and procedures for chronic wounds provides a reasonable indication of the costs that could be avoided if community health settings, including general practices, were better supported to provide evidence-based wound care. The AMA’s analysis also demonstrates that hospital admissions for chronic wounds, in particular diabetic foot ulcers, has been growing since 2015-16, and there has been an increase in hospitalisations for diabetic foot ulcers amongst younger cohorts.
This increase in younger people being hospitalised with chronic wounds has a significant impact on the health system and is demonstrative of the growing burden of disease in the community, over and above what is implied by ageing alone.
Barriers to evidence-based wound management in general practice

Research suggests that the delivery of evidence-based wound care, specifically using evidence-based practices and evidence-based wound dressings and consumables, is key to reducing the burden on patients and the healthcare system. General practices however face several barriers to delivering evidence-based wound care including inadequate funding for wound consumables, a lack of formal wound management education and training, and the absence of coordinated care pathways. In particular, the current funding arrangements do not support general practices to deliver evidence-based wound care, as the costs of providing the appropriate consumables results in a net financial loss for many general practices. Many patients are therefore required to purchase consumables from the pharmacy at retail price, or alternatively seek treatment at community healthcare settings that provide free wound care such as outpatient clinics, placing additional burden on these settings.
“Getting access to the wound dressings I need to treat my venous leg ulcer is challenging. I need to order them through the pharmacy, before visiting my regular general practitioner to have the wound assessed and dressed. The costs really add up, because it’s not just the cost of the dressings and compression bandages, it’s also the cost of specialist appointments, dermatologist appointments, travel, parking, and time off work.”
Solution to Australia’s chronic wound problem
Building on the work undertaken by the MBS Review Taskforce Wound Management Working Group, the AMA is proposing a five-point plan to improve the delivery of evidence-based wound care in general practices, which represents value to both the patient and the healthcare system.
-
A funded wound consumables scheme to subsidise the cost of wound dressings and other consumables.
Subsidised wound consumables will remove the cost barrier to accessing appropriate and evidence-based wound care products, reducing the financial strain on both patients and general practices.
It is recommended that the wound consumables scheme be initially implemented for concession and healthcare card holders, and then subsequently expanded to all patients with chronic wounds. The previous government acknowledged that general practices should not have to wear the cost of consumables and there should be "alternative sources of government support", however a funded wound consumables scheme is yet to be implemented.
The consumables scheme is estimated to cost the Commonwealth Government $3.7 million in 2022-23 ($16.1 million from 2022-23 to 2025-26) for the estimated 30 per cent of concession and healthcare card holders that would access wound care through a general practice, and $5.3 million in 2022-23 ($22.9 million from 2022-23 to 2025-26) if it was expanded to all patients.
-
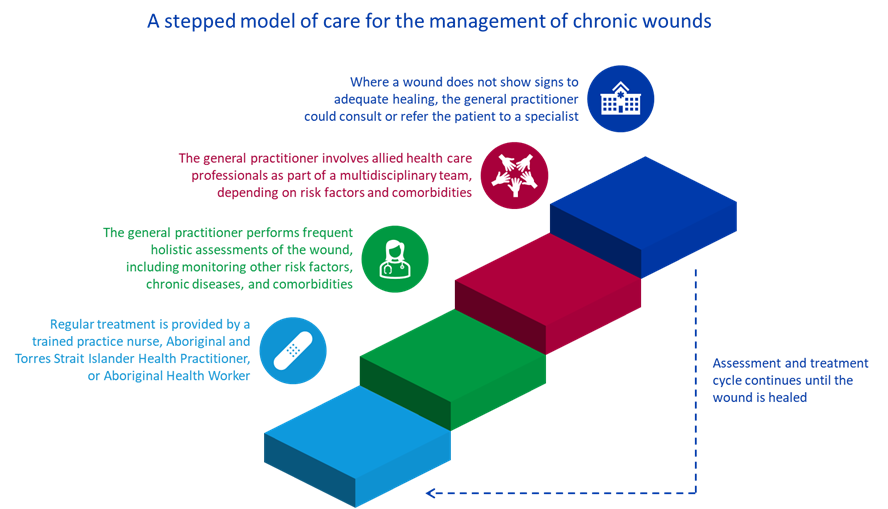
The implementation of a stepped model of care for the management of chronic wounds.
Stepped care models comprise of a hierarchy of interventions, providing patients with the least intensive intervention appropriate with regular monitoring and adjustment of treatment as required (outlined in the figure below).
As patients with chronic wounds often suffer from other chronic conditions, it is recommended that improvements be made to the current arrangements to enable practice nurses to be part of care planning for patients with chronic conditions, and better support general practitioners to employ other healthcare professionals involved in wound management, such as podiatrists, occupational therapists, dietitians, physiotherapists, orthotists, and prosthetists.
Increasing the cap on the incentive available under the Workforce Incentive Program (WIP), which will better support general practitioners to employ other healthcare professionals, is estimated to cost $48 million in 2022-23 ($207 million 2022-23 to 2025-26), and $58 million in 2022-23 ($326 million 2022-23 to 2025-26) if an annual indexation of 80 per cent Wage Price Index (WPI) and 20 per cent Consumer Price Index (CPI) is applied.
-
The creation of new wound-specific MBS items.
These new wound-specific MBS items would support general practices to assess and manage chronic wounds and facilitate the stepped model of care.
As outlined by the Wound Management Working Group, these new MBS items include:
- an item for the general practitioner to perform a comprehensive initial assessment of a chronic wound
- an item for the general practitioner to perform regular assessments of the chronic wound
- an item for an appropriately trained practice nurse, Aboriginal and Torres Strait Islander Health Practitioner, or Aboriginal Health Worker to provide short term treatment of a chronic wound.
Implementing these new MBS items is estimated to cost the government an additional $1.7 million in 2022-23 (7.4 million from 2022-23 to 2025-26). This additional cost is on top of what is already funded for the treatment of wounds through the existing MBS consultation structure and the WIP, and accounts for the proposed changes to the consultation structure. The cost however does not account for the cost of a specialist wound care practitioner. Additionally, as patients with chronic wounds often suffer from other chronic conditions and comorbidities, it is recommended that the proposed new MBS items and funded wound consumables scheme be linked to voluntary patient enrolment to support the delivery of coordinated care.
-
Implementation of a national education and training program for the management of chronic wounds.
The development of education and training requirements should be coordinated under a national program to prevent duplication and silos within the sector, and codesigned with general practitioners and other health professionals involved in the management of a chronic wound.
As recommended by the Wound Management Working Group, completion of the required education and training should be a mandatory requirement for claiming the proposed wound management MBS items and access to the wound consumables scheme.
-
Improved coordination of wound care initiatives.
The current approach to reforming the management of chronic wounds in Australia is largely piecemeal, with governments, universities, research centres, peak bodies and organisations largely taking siloed approaches to the development and implementation of wound care initiatives.
This is resulting in duplication of effort, with several initiatives and programs aimed at achieving similar outcomes currently underway.
There is an opportunity to implement a national program to coordinate the development, implementation and evaluation of programs and initiatives across all levels of the healthcare system involved in the management of chronic wounds.
Impact of evidence-based wound care
The solutions proposed represent value to both the patient and healthcare system, removing the cost barrier to accessing appropriate and evidence-based wound care products, giving patient wounds the best chance to heal. It is estimated that the delivery of evidence-based care in general practice will result in:
- Reduction in hospital admissions, with an assumed modest 20 per cent reduction resulting in an estimated saving of $19.9 million in 2022-23 ($84.9 million from 2022-23 to 2025-26).
- Reduced burden on hospital outpatient clinics (7.5 per cent of patients receiving care in hospital outpatient clinics are assumed to transition to receive care through general practices), resulting in an estimated saving of $22 million in 2022-2023 ($96.2 million from 2022-23 to 2025-26).
- Reduced burden on other community healthcare settings (2.5 per cent of patients receiving care in other healthcare settings are assumed to transition to receive care through general practices), resulting in an estimated saving of $1.4 million in 2022-2023 ($6.3 million from 2022-23 to 2025-26).
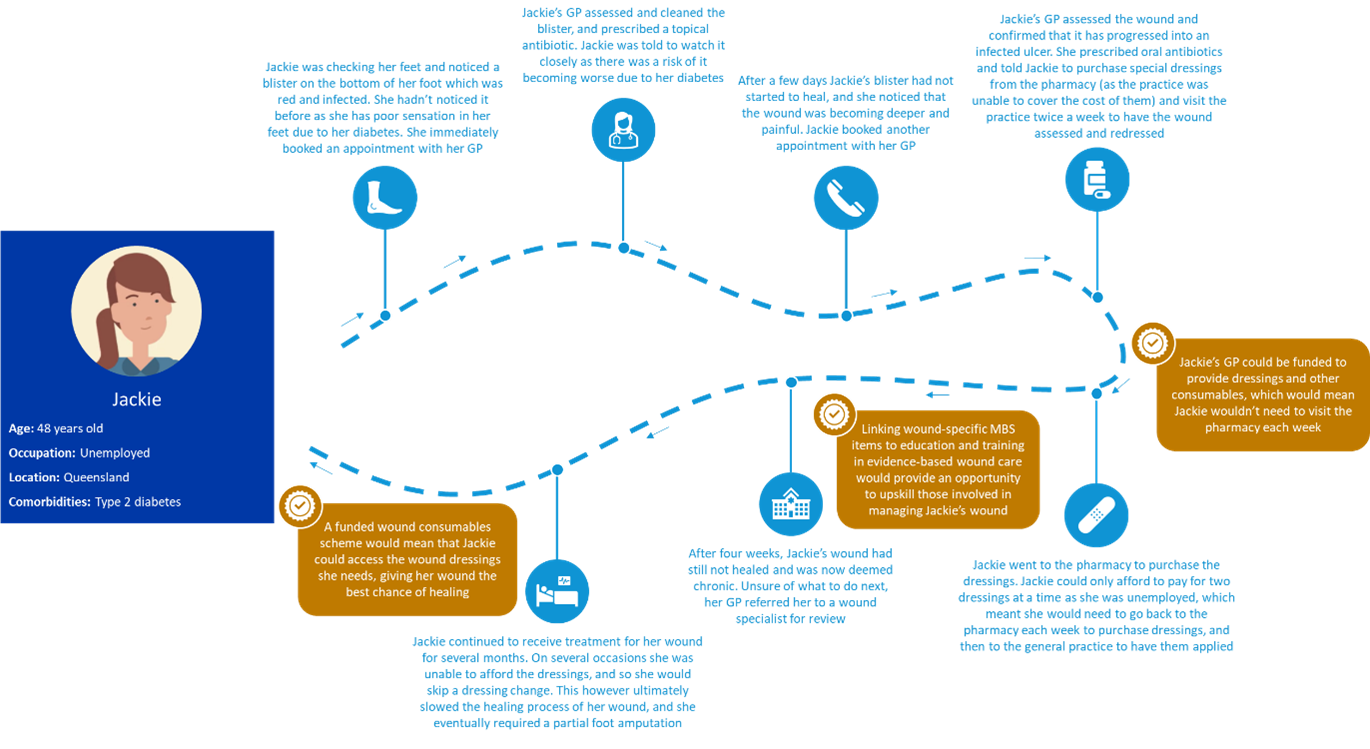
- Reduced financial burden on the patient, with the funded wound consumables scheme estimated to save patients $3.7 million in 2022-23 ($6 million from 2022-23 to 2025-26). The delivery of evidence-based care would likely reduce healing times for wounds and therefore result in further savings for the patient. Importantly, the delivery of evidence-based wound care will have a profound impact on the patient journey, saving patients both time and money, and improving health outcomes, as depicted in the figure below.
Patient journey of Jackie - a 48 year old woman with a chronic wound
The total savings for the delivery of evidence-based wound care from an assumed 20 per cent reduction in hospitalisation, savings to the consumer, and savings from transitioning a proportion of the care currently delivered in outpatient clinics and other community healthcare settings is estimated to be $47.1 million in 2022-23 ($203.4 million from 2022-23 to 2025-26).
Additionally, the proposed new MBS items are estimated to “free up” around 148,000 general practitioner consultations in the first year, and 162,000 consultations by the fourth year, as under the current consultation structure a general practitioner is required to be present on all occasions to bill the MBS.
As the program continues to expand with more chronic wounds treated in general practice, this will “free up” consultations from other healthcare settings (i.e. outpatient clinics). With Australia is now facing a serious general practitioner workforce shortage and a hospital crisis, these new MBS items will help support general practices to deliver more care to their communities and reduce the strain on public hospitals.
There is currently a disincentive for patients to receive wound care through their general practice due to the out-of-pocket costs associated with wound consumables. As patients can access free wound consumables through hospital outpatient clinics and other community healthcare settings, a funded wound consumables scheme which subsidises the cost of dressings provided in general practice will remove this disincentive. It is expected that a cost-effective wound care program that delivers evidence-based care will draw more patients over time to receive treatment at their general practice, and the amount saved would continue to increase as the proportion of wounds treated by general practice increases, depicted in the figure below.
Estimated savings from delivering evidence-based wound care in general practice
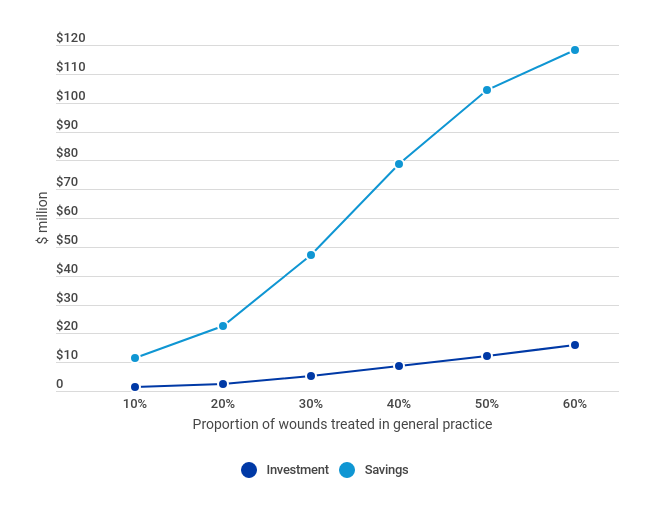
As the AMA’s modelling indicates that receiving care through the general practice is cheaper than receiving care through a hospital outpatient clinics or other community healthcare setting, it is estimated that an investment of $23.4 million in the delivery of evidence-based wound care will save the health system $203.4 million, across the forward estimates. This is a return of $8.68 for every $1.00 invested into the delivery of evidence-based wound care.