Discussion paper: Rethinking funding models to align with population health goals
As it stands today, Australia’s health system looks less and less like the system needed to care for a growing and ageing population with increased complex and chronic disease. The intent of this discussion paper is to initiate a conversation on funding reform in Australia to ensure the future sustainability of our health system.
The Australian healthcare system is regarded as one of the best in the world, however in recent years its ranking has slipped as it has struggled to adapt to meet the health needs of a changing population.
Australia is now facing several challenges that were not as prominent 50 years ago when many elements of today’s health system were established — an ageing population, chronic disease being the most dominant contemporary health issue, inequitable access to healthcare, workforce shortages, and slow adoption of new technologies.
Successive governments have sought advice on how to deal with these challenges, and successive reviews have found that the current funding arrangements contribute to creating — or at least fail to address — barriers to coordinated, patient-centred, and effective healthcare that is delivered in the most cost-effective setting.
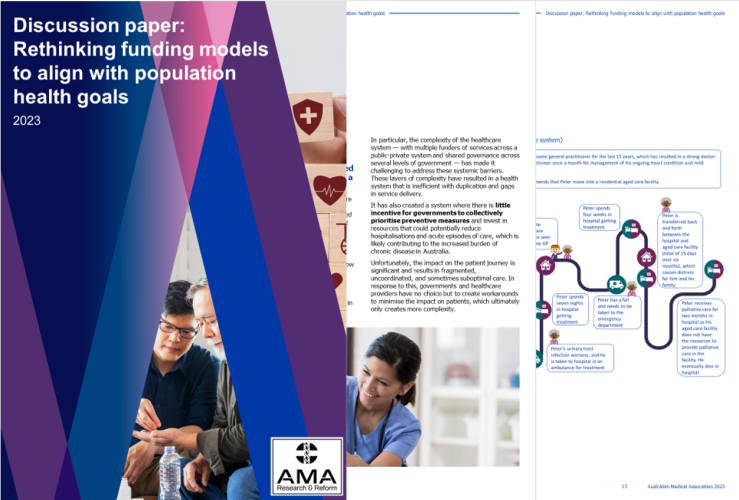
In particular, the complexity of the healthcare system — with multiple funders of services across a public-private system and shared governance across several levels of government — has made it challenging to address these systemic barriers. These layers of complexity have resulted in a health system that is inefficient with duplication and gaps in service delivery.
It has also created a system where there is little incentive for governments to collectively prioritise preventive measures and invest in resources that could potentially reduce hospitalisations and acute episodes of care, which is likely contributing to the increased burden of chronic disease in Australia.
Unfortunately, the impact on the patient journey is significant and results in fragmented, uncoordinated, and sometimes suboptimal care. In response to this, governments and healthcare providers have no choice but to create workarounds to minimise the impact on patients, which ultimately only creates more complexity.
As it stands today, Australia’s health system looks less and less like the system needed to care for a growing and ageing population with increased complex and chronic disease.
A significant change in the funding arrangements is needed to ensure the sustainability of our health system. This will require funding models that not only tackle existing health issues, but incentivise funders to prioritise prevention and early intervention to reduce acute and more costly care in the long-term, particularly for populations who are at risk of needing acute care. An example of such a funding model is a single-payer funding model, where a single entity, often a government, is responsible for funding the delivery of healthcare for a targeted population.
Transiting the current healthcare system to a single-payer model would require radical health system reform and it is unlikely the benefits from this transition would outweigh the costs and effort to redesign the system. Analysis of single-payer case studies however reveals it may be worthwhile considering single-payer models or other types of innovative funding reform for targeted populations, particularly those that experience increased burden of chronic disease and high potentially preventable hospital admissions.
One population that could benefit from new and innovate funding models is older Australians (65 years and older), as they are estimated to account for almost half (46 per cent) of preventable hospitalisations and have a high burden of chronic disease.
The AMA's analysis reveals new funding models that incentivise the avoidance of preventable hospital admissions and readmissions for older Australians could save up to $31.49 billion over the forward estimates (2024–25 to 2027–28). This type of funding model could also be extended more broadly to populations with chronic and complex diseases, as well as diverse populations, as these cohorts also experience high preventable hospital admissions and readmissions. These patients would also benefit from some of the other benefits of single-payer models, such as the delivery of more coordinated, patient-centred, and efficient care.
While a single-payer funding model does not guarantee more cost-effective and coordinated healthcare, it is undeniably an elegant approach to incentivise behaviour that could lead to achieving such outcomes. It is however important to acknowledge there are various mixed funding health systems worldwide that have delivered cost-effective, coordinated and patient-centred care. Single-payer funding models for targeted populations is an example of funding reform that holds promise, as it would incentivise a focus on prevention and early intervention, ultimately promoting improved health outcomes for these populations. There are however other innovative funding models that could achieve these outcomes, and the intent of this discussion paper is to initiate the conversation on funding reform in Australia to ensure the future sustainability of our health system.



