2024 Public hospital report card - mental health
edition
State by state public hospital performance - Victoria
Mental health capacity in public hospitals
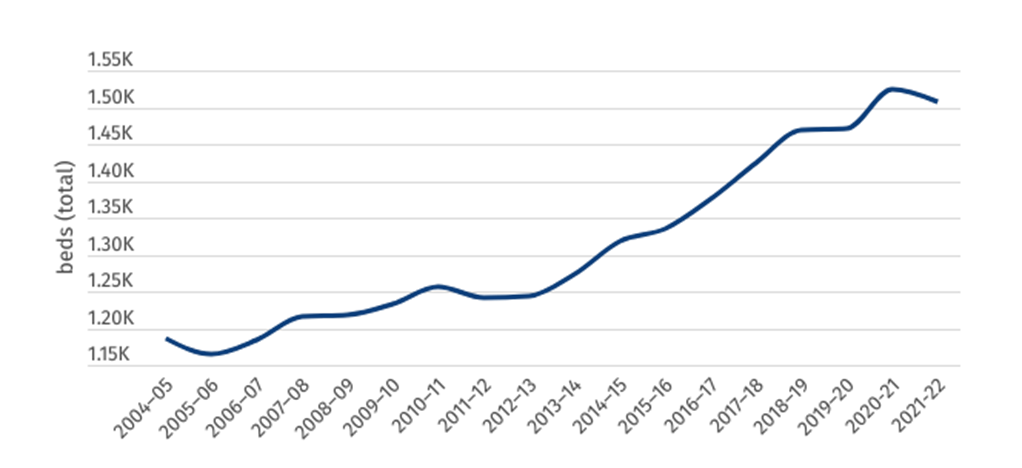
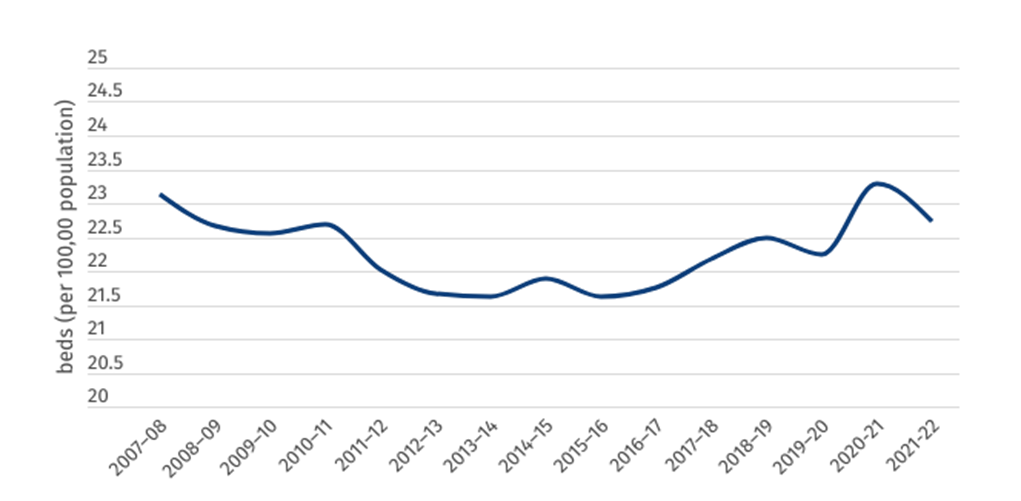
Victoria has been increasing the number of specialised mental health public hospital beds at a nation-leading rate for the past 10 years, with the total number of public sector specialised mental health hospital beds increasing from 1241 to 1507 since 2011–12. However, this increase has been almost entirely offset by an increasing population, with the number of beds available per 100,000 Victorians increasing only slightly over this time.
Victoria’s 23 beds per 100,00 sits well below the national average of 27 beds per 100,000, indicating further investment is vitally necessary to provide Victoria’s public hospitals with the capacity to sufficiently treat those suffering from acute mental health problems.
Figure 1: Total number of specialised mental health public hospital beds (Vic)
Figure 2: Specialised mental health public hospital beds per 100,000 population (Vic)
Mental health presentations to ED
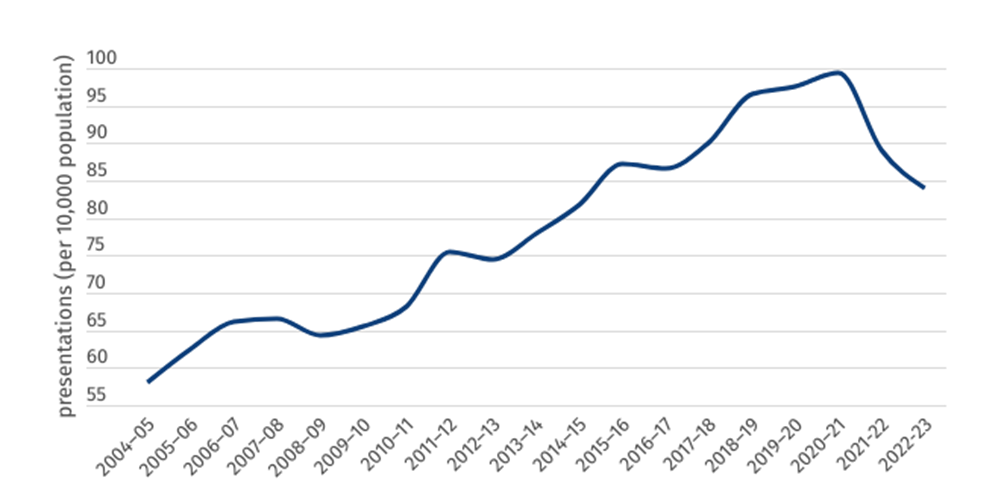
The number of per-population mental health presentations fell slightly in 2022–23, from 89 per 10,000 to 84 per 10,000 in Victoria. This is the lowest per-person rate in any Australian jurisdiction, even as the severity of presentations to ED continues to rise.
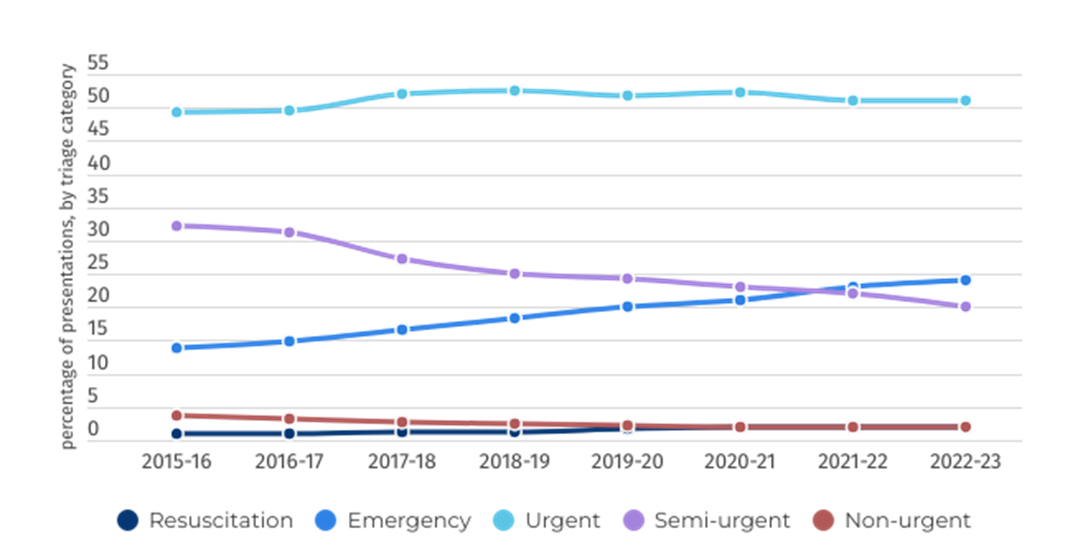
As shown in figure 4, the most frequent triage category for patients presenting to hospital with a mental health condition remains triage category 3, “urgent”, meaning the patient should be seen within 30 minutes. Worryingly, the share of patients triaged as “emergency” (within 10 minutes) has become the second most common presentation type, rising from 14 per cent of presentations in 2015–16 to 24 per cent in 2022–23
Figure 3: Rate of ED mental health presentations per 10,000 population (Vic)
Figure 4: Mental health-related ED presentations, by triage category, per cent (Vic)
Length of stay
This page demonstrates the length of stay for mental health patients across two areas of the public hospital — the emergency department and inpatient beds once admitted to hospital.
Mirroring national trends, Victoria has seen a worrying and consistent increase in the median time spent in emergency departments. Patients who are eventually admitted to hospital are spending, on average, more than two hours longer in emergency departments than they were just five years prior. Ten per cent of patients now wait 22 and a half hours in an overcrowded and stressful ED due to poorly resourced and over capacity hospitals.
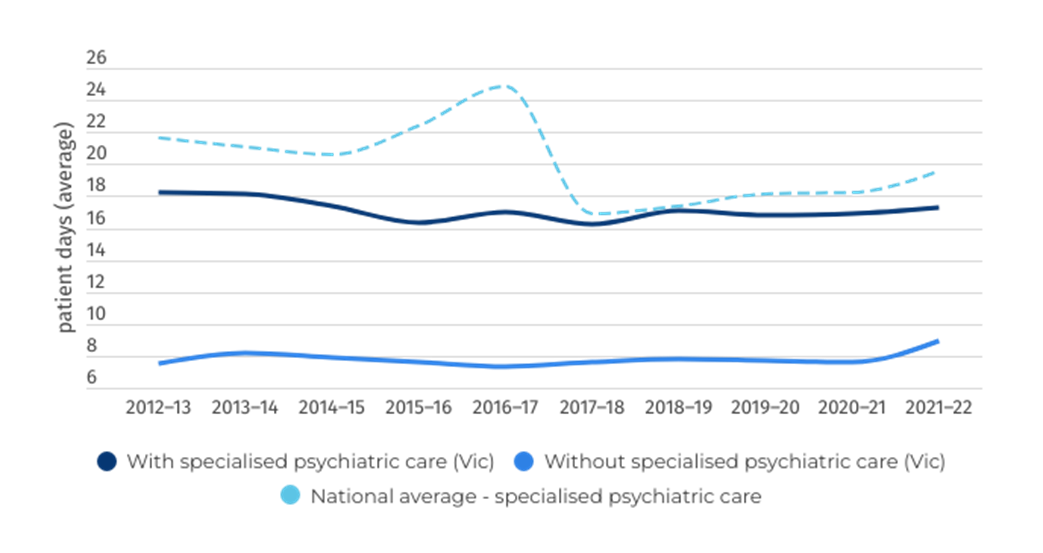
Figure 6 shows the average length of stay for admitted overnight mental health patients receiving specialised psychiatric care is below the national average, at 17.24 days in 2021–22.
Figure 5: Length of Stay in ED (Vic)
Figure 6: Overnight admitted care length of stay (days) (Vic)
Clinical outcomes
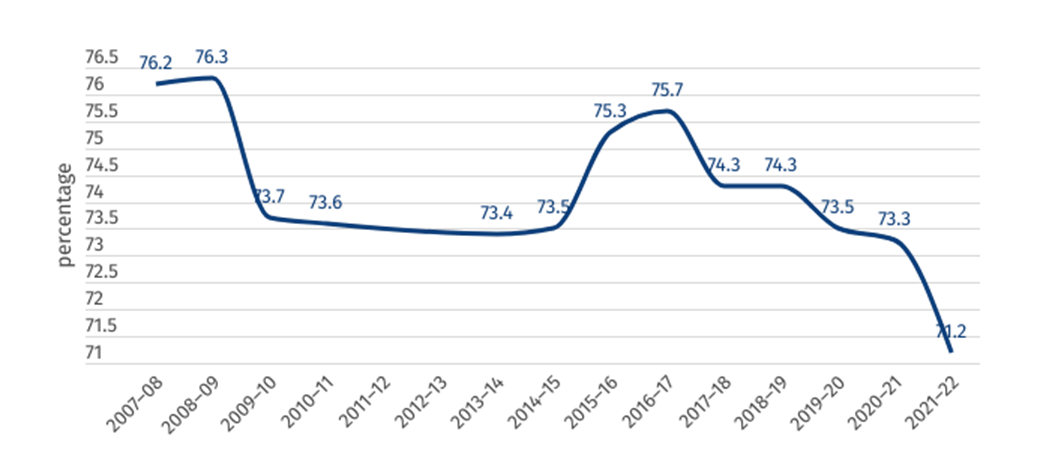
Figure 7 shows the percentage of mental health inpatients who saw a significant improvement to their clinical outcome according to the National Outcomes and Casemix Collection (NOCC). While these figures should not be compared across jurisdictions, 71.2 per cent of mental health-related public hospital inpatients surveyed saw a significant improvement as a result of their treatment in 2021–22 across Victoria, the lowest result in the past 15 years. Note that data is missing for the period from 2011 to 2013.
Figure 7: Clinical outcome of people receiving mental healthcare in hospital (percentage who saw a significant improvement)
Community follow-up
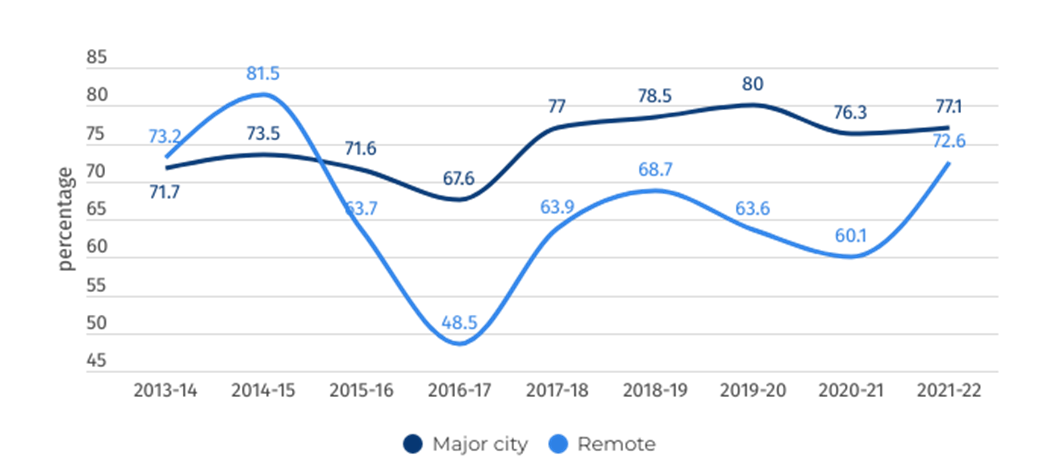
Community follow-up after psychiatric admission/hospitalisation is defined as the proportion of state and territory governments’ specialised public admitted patient overnight acute separations from psychiatric units for which a community-based ambulatory contact was recorded in the seven days following separation.
Figure 8: Rate of community follow up within 7 days of discharge from a psychiatric admission